The HPV Vaccine is Underutilized–And How We Can Change That
September 18, 2019 by Justin Lehmiller
The human papillomavirus (HPV) is the most common sexually transmitted infection and it’s responsible for a number of negative health effects. In addition to genital warts, it has the potential to cause a number of cancers, including those of the cervix, anus, and throat. A vaccine that can prevent HPV (and, therefore, its associated health problems) has been around for nearly a decade; however, it continues to be widely underutilized in the United States.
The HPV vaccine is most effective if administered in childhood before sexual activity begins and, thus, before any potential HPV exposure. While more parents are opting to have their kids vaccinated than ever, there are still millions who are going without and who will therefore be at risk for infection later in life. Specifically, what the latest data show is that just a bare majority—51.1%—of adolescents aged 13-17 are up to date on the vaccine series, which involves two to three shots administered over a period of several months. A larger number (68.1%) have received at least one shot; however, to get maximum protection for any vaccine, all required doses must be received.
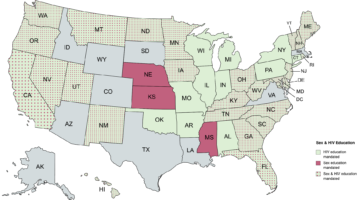
Vaccination rates for adolescents vary widely across the country. For example, in some states—such as Texas, Indiana, South Carolina, and Kentucky—fewer than half of adolescents have received the vaccine. By contrast, in California, New York, and Massachusetts, more than 70% have received at least one dose. In other words, there’s even more room for improvement in some parts of the US.
In order to increase vaccination rates, we need to do a few things. First, we need to combat persistent myths and misconceptions, such as the claim that this vaccine poses serious health risks. The truth is that this vaccine is safe and effective, and no riskier than other vaccines [1]. Likewise, some people have expressed concerns about whether this vaccine will increase rates of risky sexual behavior; however, research has not found any support for that idea [2]. Adolescents aren’t making sexual decisions based on whether they’ve received this vaccine.
Second, physicians need better education about this vaccine because it turns out that many of them are engaging in behaviors that are discouraging teens from receiving it, such as not giving timely vaccine recommendations, failing to recommend same-day vaccination, and only recommending it to those deemed “at risk” [3].
Third, we need to get policy makers on board. There is a lot that states can do legislatively that have the potential to help, such as by creating policies that increase HPV awareness and that encourage vaccination. Efforts to mandate this vaccine have proved controversial; however, if politicians can at least work toward increasing awareness of HPV and reducing barriers to vaccination, that would be a big step in the right direction.
Lastly, it’s important to note that the HPV vaccine isn’t just for kids. Adults—who are even less likely to be vaccinated—can potentially benefit from it, too. Although this vaccine used to only be recommended for persons up to age 26, the recommended age has recently been expanded to 45. This doesn’t necessarily mean that effectiveness stops at 45—persons over that age can still get the vaccine and potentially benefit from it. The only issues are that insurance companies are unlikely to cover it if you’re over the recommend age and the vaccine may not provide as much protection (people who have been sexually active for a longer period of time are more likely to have already been exposed to some strains of HPV). That said, the point here is that we need to increase awareness of this vaccine beyond parents because it’s not just kids who will benefit from receiving it.
Want to learn more about Sex and Psychology ? Click here for previous articles or follow the blog on Facebook (facebook.com/psychologyofsex), Twitter (@JustinLehmiller), or Reddit (reddit.com/r/psychologyofsex) to receive updates. You can also follow Dr. Lehmiller on YouTube and Instagram.
[1] Reiter, P. L., Brewer, N. T., Gottlieb, S. L., McRee, A. L., & Smith, J. S. (2009). How much will it hurt? HPV vaccine side effects and influence on completion of the three-dose regimen. Vaccine, 27(49), 6840-6844.
[2] Smith, L. M., Kaufman, J. S., Strumpf, E. C., & Lévesque, L. E. (2015). Effect of human papillomavirus (HPV) vaccination on clinical indicators of sexual behaviour among adolescent girls: the Ontario Grade 8 HPV Vaccine Cohort Study. Canadian Medical Association Journal, 187(2), E74-E81.
[3] Gilkey, M.B. et al. (2015). Quality of physician communication about human papillomavirus vaccine: Findings from a national survey. Cancer Epidemiology, Biomarkers & Prevention. doi: 10.1158/1055-9965.EPI-15-0326
Image Source: 123RF/Supak Katedee

Dr. Justin Lehmiller
Founder & Owner of Sex and PsychologyDr. Justin Lehmiller is a social psychologist and Research Fellow at The Kinsey Institute. He runs the Sex and Psychology blog and podcast and is author of the popular book Tell Me What You Want. Dr. Lehmiller is an award-winning educator, and a prolific researcher who has published more than 50 academic works.
Read full bio >